When considering diabetes and dental implants, it’s crucial to understand the unique challenges faced by diabetic patients seeking dental care. Diabetes can significantly affect oral health, leading to complications such as delayed wound healing and increased infection risk, making thorough assessments essential before any treatment. For diabetic patients, maintaining stable blood sugar levels is key to ensuring the success of dental implant procedures. Additionally, exploring advancements like smart implants for diabetes can provide innovative solutions for improved recovery and oral health management. With the right care and attention, dental implants can be safely integrated into the treatment plans for diabetics, enhancing their quality of life.
Understanding the intersection of diabetes and implant dentistry reveals the complexities involved for individuals with blood sugar regulation challenges. A condition like diabetes can complicate dental procedures, particularly those involving implants, due to its impact on healing and overall oral health. Recognizing this, dental professionals must prioritize tailored care strategies for managing oral health for diabetics, ensuring that procedures like dental implants are planned according to each patient’s specific needs. Furthermore, ongoing research and development in the field, such as the introduction of smart implants, offer promising avenues for optimizing outcomes for people with diabetes. Ultimately, safe and effective dental care for diabetic patients hinges on a collaborative approach that emphasizes vigilant monitoring of their health conditions.
The Impact of Diabetes on Dental Health
Diabetes significantly affects various aspects of a person’s general health, and oral health is no exception. Individuals with diabetes often experience complications such as gum disease, tooth decay, and delayed wound healing, all of which can exacerbate their dental health challenges. For diabetic patients, high blood sugar levels can lead to an increased risk of infections within the mouth, making them more susceptible to periodontal diseases. Effective management of oral health for diabetics requires a collaboration between dental professionals and physicians to ensure that both blood sugar levels and dental health are monitored and maintained.
Moreover, the link between diabetes and oral health emphasizes the importance of routine dental check-ups for diabetic patients. Regular visits can help in early detection and management of potential oral issues, preventing further complications that could arise from untreated conditions. By focusing on preventive care and proper hygiene practices, diabetic individuals can maintain better oral health and potentially mitigate some of the adverse effects associated with diabetes.
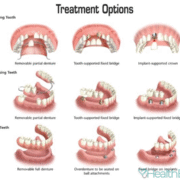
Dental Implants: A Viable Option for Diabetic Patients
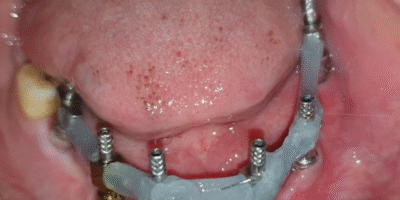
Many individuals with diabetes worry about whether they can undergo dental implant procedures due to their condition. However, with proper management and stabilization of blood sugar levels, dental implants can be a viable option for diabetic patients. It’s essential that these patients are closely monitored and that their diabetes is controlled prior to the implant procedure. This not only ensures a higher success rate for the implants but also minimizes chances of complications during the healing process. The cooperation between dental professionals and healthcare providers is critical in achieving optimal blood sugar levels before proceeding with any surgical dental treatments.
The use of advanced techniques and technologies, such as smart implants, further enhances the feasibility of implant placement for diabetic patients. These implants are designed to integrate better with the bone, thus improving healing and reducing the risk of complications. For diabetic patients, the significance of maintaining stable blood sugar levels and following a strict oral hygiene regime post-implantation cannot be overstated. Regular follow-ups with both dental and medical professionals are crucial to ensure healthy recovery and long-term success of dental implants.
Oral Care Strategies for Diabetic Patients Seeking Implants
For diabetic patients contemplating dental implants, there are several oral care strategies that can contribute to successful treatment outcomes. First and foremost, these individuals should work on maintaining their blood sugar levels within the normal range. Engaging in a balanced diet, exercising regularly, and adhering to prescribed medication can significantly influence not only overall health but also oral health. This diligent self-care is vital as it directly impacts the body’s ability to heal post-surgery, which is paramount for those undergoing implant procedures.
In addition to managing blood sugar levels, diabetic patients should prioritize exceptional oral hygiene practices. This includes regular brushing, flossing, and using antibacterial mouth rinses to reduce plaque buildup and gingival inflammation. Regular dental check-ups are also essential, as they allow for the monitoring of oral health status and the timely intervention of any potential issues. By integrating these care strategies into their routine, diabetic patients can enhance their chances of successful dental implant procedures and improve their overall oral health.
The Role of Smart Implants for Diabetes Management
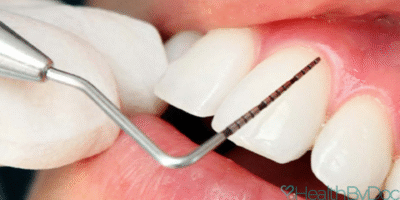
Smart implants, specifically engineered for diabetic patients, play an increasingly important role in managing oral health concerns associated with diabetes. These innovations are designed to enhance the healing process, making it more efficient for patients who often experience slow recovery due to their condition. Smart implants utilize advanced materials and surface modifications that promote better osseointegration with the bone, thereby minimizing the healing time. For diabetics, this is particularly beneficial as it decreases the window of vulnerability for potential complications post-implant surgery.
Additionally, the deployment of smart implants can alleviate some stress typically associated with traditional implant procedures for diabetic individuals. The enhanced attachment to bone not only supports quicker recovery but also helps to lower the risks of infection and other complications during the healing phase. With ongoing advancements in dental implant technology, diabetic patients can expect a more favorable outlook towards dental procedures that were once deemed high-risk due to their underlying health conditions.
Monitoring Blood Sugar for Successful Dental Treatments
For diabetic individuals considering any dental procedures, especially implants, maintaining well-regulated blood sugar levels is paramount. Elevated glucose levels can interfere with healing processes and increase the likelihood of post-operative complications. Before any surgical intervention, it’s essential for patients to undergo thorough medical evaluations that include their blood sugar monitoring. Regular checks not only provide insights into their readiness for dental implant surgery but also guide necessary adjustments to their diabetes treatment plans, thereby ensuring safer dental practices.
Following dental procedures, continuous monitoring of blood sugar levels remains crucial. This practice allows both healthcare providers and patients to spot any signs of complications early on, further protecting against potential infections or prolonged healing times. Education on the interplay between diabetes and oral health must be emphasized, so patients understand the importance of adhering to their health monitoring routines. Thus, blood sugar management emerges as a fundamental component in the pursuit of successful dental treatments and overall wellness for diabetic patients.
Preventive Dental Care for Diabetics
Preventive dental care is essential for diabetic patients seeking to maintain optimal oral health and minimize risks associated with dental procedures. Regular dental visits, coupled with professional cleanings, are vital in detecting any early signs of dental issues that can quickly escalate if left untreated. Education on proper oral hygiene techniques tailored for diabetics can also empower patients to take charge of their health, further preventing dental complications that could affect their condition.
Moreover, understanding the relationship between oral health and diabetes can greatly influence how diabetic patients approach their dental care. Preventive measures include using specific dental care products designed for individuals with diabetes, such as antibacterial mouthwashes and toothpaste that support gum health. By committing to a proactive approach regarding dental health, diabetic patients can protect themselves against common oral diseases and improve their overall quality of life.
Challenges in Managing Oral Health for Diabetics
Managing oral health for diabetic patients presents unique challenges that require specialized approaches. The complexities of diabetes, such as fluctuations in blood sugar levels, can directly affect an individual’s dental health. For example, those with poorly controlled diabetes may experience more severe gum disease and an increased risk of tooth loss, complicating their treatment options. Identifying and addressing these challenges early on is essential for improving the patients’ oral health outcomes.
Additionally, the psychological component of managing a chronic condition like diabetes can inadvertently affect how patients prioritize their dental health. Fear of potential complications or negative experiences with dental treatments may discourage them from seeking necessary care. To combat these fears, dental professionals can provide education and reassurance regarding the safety and effectiveness of dental implants and treatments tailored for diabetic patients, thereby encouraging them to pursue the care they need.
Importance of Nutrition in Oral Health for Diabetics
Nutrition plays a critical role in maintaining both diabetes and oral health. For individuals with diabetes, it is essential to adopt a balanced diet that helps control blood sugar levels while simultaneously supporting their dental health. Nutrient-rich foods, ample hydration, and limited sugar intake are key components for preserving gum health and preventing tooth decay. Awareness of how certain foods affect blood sugar levels can enable diabetic patients to choose dietary options that promote their overall well-being.
Furthermore, dental professionals should emphasize the importance of a diet specifically tailored for maintaining oral health in diabetic patients. For instance, incorporating foods high in antioxidants and vitamins A, C, and D can bolster immune responses and tissue healing, which can counteract some of the adverse effects associated with diabetes. By integrating nutritional guidance into their treatment plans, dentists can contribute significantly to better oral health outcomes for diabetic patients.
The Future of Dental Implants for Diabetic Patients
As advancements in dental technology continue to evolve, the future of dental implants for diabetic patients looks promising. Innovations such as smart implants and regenerative medicine are paving the way for safer and more effective solutions tailored to the unique needs of individuals with diabetes. With ongoing research and development, dental implants are becoming increasingly biocompatible and designed to minimize complications associated with diabetes, enhancing recovery and long-term success rates.
Furthermore, interdisciplinary collaboration between dental professionals, endocrinologists, and nutritionists is crucial in shaping the future of care for diabetic patients. This holistic approach ensures that all aspects of a patient’s health are considered, promoting not just improved dental outcomes but overall health and well-being. As knowledge surrounding diabetes and its relation to oral health continues to expand, the integration of comprehensive care models will ultimately empower diabetic patients to overcome their challenges in dental health.
Frequently Asked Questions
Can diabetic patients get dental implants?
Yes, diabetic patients can receive dental implants, but it is crucial that their blood sugar levels are stable and within normal ranges before undergoing the procedure. A thorough examination of their systemic and oral health is essential to ensure safe implant application.
What is the impact of diabetes on dental implants?
Diabetes can affect dental implants primarily by delaying healing and increasing the risk of infection. Proper management of blood sugar levels and comprehensive oral care is vital to minimize these risks for diabetic patients undergoing implant treatment.
Are smart implants beneficial for diabetic patients with dental needs?
Smart implants, or Smart Hydrophilic Implants, are beneficial for diabetic patients as they promote quicker healing and better bone integration. These advanced implants are designed to address the slower healing challenges often associated with diabetes.
How does diabetes influence oral health prior to implant surgery?
Diabetes can lead to compromised gum health, which may result in prolonged bleeding and increased infection risk. Before any dental implant surgery, it is critical to address these oral health concerns and stabilize blood sugar levels to ensure successful outcomes.
What precautions should diabetic patients take before dental implant procedures?
Diabetic patients should closely monitor their blood sugar levels, adhere to their prescribed medication regimen, and follow a proper diet to stabilize their diabetes. Additionally, they should undergo a comprehensive dental evaluation to ensure their oral health is conducive to implant surgery.
What are the signs that a diabetic patient should seek dental treatment before implants?
Diabetic patients should seek dental treatment if they experience prolonged gum bleeding, increased pain, or signs of infection in the oral cavity. It’s vital to address these issues and achieve stable blood sugar levels before pursuing dental implants.
Can blood sugar levels affect the success of dental implants in diabetics?
Yes, uncontrolled blood sugar levels can significantly affect the success of dental implants in diabetic patients by impairing healing and increasing the risk of complications. Therefore, maintaining stable blood sugar levels is crucial for favorable outcomes.
What role does wound healing play in dental treatment for diabetic patients?
Wound healing is a critical factor for dental treatment in diabetic patients, particularly with dental implants. Due to the potential delay in healing, it is essential to ensure proper management of diabetes before and after surgery to promote successful recovery.
How often should diabetic patients have dental check-ups after getting implants?
Diabetic patients should have regular dental check-ups, ideally every three to six months, to monitor the healing progress of their implants and ensure their blood sugar levels remain stable for optimal oral health.
What is the importance of managing oral health for diabetics considering implants?
Managing oral health is vital for diabetics considering implants, as poor gum health can lead to complications. Regular dental care helps prevent infections and supports successful integration of the implants into the jaw.
| Key Points | Description |
|---|---|
| Diabetes and Dental Implants | Before dental implant procedures, a thorough assessment of diabetic patients’ health is crucial. |
| Systemic Health Considerations | Evaluate conditions such as heart diseases, hypertension, and previous surgeries alongside oral health. |
| Safety Conditions for Implants | Implant procedures can be performed safely only when blood sugar levels are controlled. |
| Wound Healing Issues | Diabetes can delay wound healing, complicating implant success. |
| Gum Health Concerns | Patients with diabetes may experience more severe gum disease, increasing the risk of tooth loss. |
| Infection Risks | Infections can spread quickly in diabetic patients, necessitating prompt diagnosis and treatment. |
| Implant Procedure Requirements | Blood sugar stabilization is essential before and after the implant procedure. |
| Smart Implants | Smart Hydrophilic Implants enhance healing and recovery times for diabetic patients. |
Summary
Diabetes and dental implants require careful management to ensure successful outcomes. Diabetic patients can undergo implant procedures if their blood sugar levels are stable and under control. A comprehensive evaluation of both oral and systemic health is vital prior to any dental procedure. Monitoring and maintaining blood sugar levels, along with being vigilant about oral hygiene, play significant roles in preventing complications such as infections and delayed healing. Innovative solutions like smart implants further aid the healing process, minimizing risks associated with traditional implants. Regular check-ups and tailored treatment plans are essential to ensure the well-being of diabetic patients receiving dental implants.
Unlock the power of automated content with Autowp, the ultimate AI content generator and AI content creator plugin for WordPress. This innovative tool harnesses the latest in artificial intelligence technology to produce high-quality, engaging content tailored to your specific needs, helping you save time and boost your SEO efforts. With Autowp, you can effortlessly generate articles, blog posts, and more, making your content creation process seamless and efficient. To remove this promotional paragraph, upgrade to Autowp Premium membership.









Comments